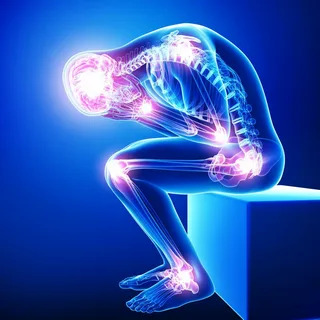
The complicated and difficult condition of chronic pain can have a major negative effect on a person’s quality of life. Although pain management is important, the purpose of treatment goes beyond symptom relief. The goals of transformative therapies are to create long-lasting alleviation, enhance general wellbeing, and address the underlying causes of pain. This post will discuss novel, all-encompassing methods of treating pain that concentrate on transformation and healing rather than just treating symptoms.
Comprehending Chronic Pain
Persistent discomfort that lasts for a long time—usually longer than the anticipated time for tissue healing—defines chronic pain. It can be caused by a number of things, such as musculoskeletal problems, medical disorders, traumas, or nerve damage. In contrast to acute pain, which acts as a defense mechanism, chronic pain can worsen and impair one’s ability to operate physically, emotionally, and generally.
The Effects of Long-Term Pain
Beyond just being uncomfortable physically, chronic pain can have a significant impact on many facets of life.
Emotional Well-Being:
Depression, anxiety, stress, and mood disorders are frequently linked to chronic pain, which can result in emotional suffering and a lower quality of life.
Physical Functioning: Prolonged pain might make it difficult to move around, impede one’s ability to perform everyday tasks, work, or engage in leisure activities.
Sleep Disturbances:
Pain-related sleep disturbances can make pain, exhaustion, and cognitive impairments worse. Examples of these disturbances include insomnia and irregular sleep patterns.
Social and Interpersonal Relationships: Relationships can be strained, social isolation can be exacerbated, and social interactions and support networks can be impacted by chronic pain.
Revolutionary Therapies for Prolonged Relief
Chronic pain must be treated with a multimodal, integrated strategy that addresses the physical, psychological, and behavioral elements that affect how pain is perceived and managed in addition to focusing on the underlying mechanisms causing the pain. The following revolutionary therapies provide long-lasting relief:
1. Thorough Pain Evaluation
Healthcare professionals must do a comprehensive examination in order to determine the kind, degree, underlying causes, and effects of pain on a person’s life. This evaluation could consist of:
Medical History:
Recording past trauma, illnesses, surgeries, prescription drugs, and pain management procedures.
Physical examination: Assessing range of motion, neurological symptoms, musculoskeletal function, and sensitive or sore spots.
Diagnostic testing:
To find anatomical or functional anomalies causing pain, researchers use imaging investigations, nerve conduction tests, blood tests, and other diagnostic instruments.
Assessing pain’s severity, quality, duration, triggers, aggravating circumstances, and effects on everyday activities, mood, and sleep is done by using validated pain questionnaires.
2. The Multidisciplinary Approach to Treatment
A thorough and coordinated approach to pain treatment is ensured by collaborative care, which involves a team of healthcare experts from diverse disciplines. This interdisciplinary group could consist of:
Pain medicine specialists are medical professionals with a focus on managing pain who evaluate, identify, and create treatment regimens for persistent pain disorders.
Physical therapists are specialists in pain management and rehabilitation who create individualized exercise plans, manual therapies, and other techniques to increase strength, mobility, and relieve pain.
Psychiatrists and psychologists are mental health providers who address the emotional component of pain by offering coping mechanisms, mindfulness-based interventions, relaxation methods, and cognitive-behavioral therapy (CBT).
Practitioners of Complementary Medicine:
Professionals who provide complementary therapies like massage therapy, herbal medicines, acupuncture, chiropractic adjustments, and mind-body techniques to improve general well-being and pain alleviation.
3. Specific Pain Management
Novel and focused pain therapies try to target particular systems that underlie chronic pain, such as:
Neuromodulation Therapies:
Electrical impulses are delivered by methods including spinal cord stimulation (SCS), peripheral nerve stimulation (PNS), and deep brain stimulation (DBS) to modify pain signals and alleviate some chronic pain problems.
Injections and Blocks: Local anesthetics, botulinum toxin, or corticosteroids can be injected specifically into painful sites to decrease inflammation, block pain signals, and relieve symptoms.
Regenerative medicine:
New treatments include stem cell therapy, platelet-rich plasma (PRP) injections, and regenerative tissue grafts seek to restore function, lessen inflammation, and encourage tissue healing in deteriorated or injured tissues that cause pain.
Medical gadgets:
Non-invasive choices for pain management, relaxation, distraction, and rehabilitation are provided by cutting-edge gadgets like wearable technology, biofeedback devices, and virtual reality systems.
Pharmacogenomics: Using genetic testing to find genetic variants that may affect how the body reacts to painkillers, pharmacogenomics is a personalized medicine method that enables the development of individualized and successful pharmacological therapies.
4. Optimization of Lifestyle
Improving lifestyle variables can be very helpful in controlling chronic pain and enhancing general wellbeing:
Physical Activity:
By releasing endorphins and other naturally occurring painkillers, frequent exercise, stretching, and movement treatments can enhance cardiovascular health, muscle strength, joint flexibility, and pain regulation.
Nutrition:
Eating a well-balanced diet high in antioxidants, vitamins, minerals, and anti-inflammatory foods promotes tissue healing, lowers inflammation, and improves resilience and general health.
Sleep hygiene can help to enhance sleep quality, lessen pain-related sleep disturbances, and speed up recovery. It involves establishing healthy sleep habits, establishing a restful nighttime routine, optimizing the sleep environment, and treating sleep disorders.
Stress Management:
You can reduce stress, ease tension in your muscles, and enhance your ability to cope with pain by engaging in stress-relieving activities including deep breathing, mindfulness meditation, relaxation exercises, and hobbies.
5. Self-care, Empowerment, and Education
Long-term success depends on providing people with the information, abilities, and tools they need to take care of themselves and manage their pain:
Patient education
Giving people thorough knowledge about pain issues, available treatments, coping mechanisms, self-care practices, and community resources enables them to take an active role in their care and make wise decisions.
Self-Care behaviors:
Resilience, self-efficacy, and well-being are enhanced by supporting self-care behaviors such as goal-setting, pacing activities, self-monitoring, using assistive technology, practicing relaxation techniques, and preserving social relationships.
Peer Assistance and Local Resources:
Facilitating access to peer support groups, online forums, educational workshops, and community resources for those with chronic pain can reduce feelings of isolation and promote resilience by fostering social connection, validation, empathy, and shared experiences.
In summary
Beyond merely managing symptoms, transformative therapies for chronic pain try to address the underlying causes of the condition, enhance general wellbeing, and foster resilience and long-lasting alleviation. People with chronic pain can experience transformation, healing, and a renewed sense of control and vitality in their lives by adopting a comprehensive and integrated approach that combines cutting-edge therapies, multidisciplinary care, lifestyle optimization, education, empowerment, and self-care practices.